The omega loop gastric bypass (mini-loop gastric bypass)
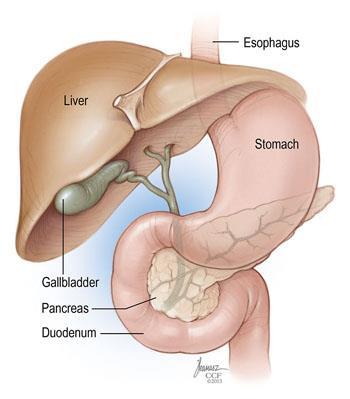
The Omega Loop is the reduction in the size of your stomach and re-arrangement of your small
bowel such that the mixing of digestive enzymes / bile (required for the breakdown of
calories / vitamins) with swallowed food is delayed (bypassed) to decrease absorption. This
results in respective restrictive and malabsorptive changes that results in weight loss and
generally improvement in various comorbidities (such as diabetes and hypertension).
An Omega loop Bypass is a major laparoscopic operation, and requires lifestyle changes to
maximise its results.
How does an Omega Loop Gastric Bypass work?
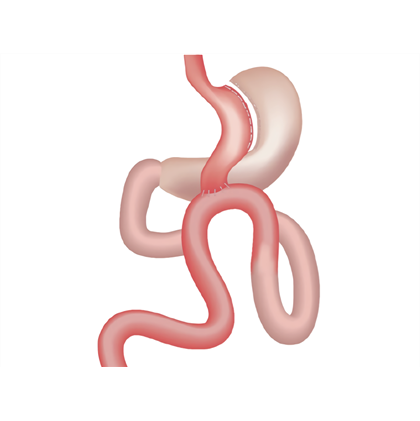
Restrictive
The majority of the stomach is removed. Approximately 100- 150ml 'sleeve' of stomach remains
(<10% of stomach). This results in 'early satiety' , this is the sensation of feeling
full
and satisfied after eating smaller volumes and thus less calories eaten through
regulation of hormones ("Ghrelin").
Malabsorptive
This pouch is reconnected to a segment of small bowel in a "loop" configuration
resulting in the nutrients eaten not being in contact with the enzymes required for
breakdown and digestion until further down the gastrointestinal tract (The "gut")
than normal. Therefore the body has less time to absorb these calories before
passage into the large bowel / colon
Other Changes
Metabolic changes occur after the operation. These are changes in the hormones and
signals sent from the remaining stomach to the body. These signals cause the body to
secrete less hormones, that in turn 'turn down' your appetite. Your body responds by
controlling glucose and fats better within the blood stream. Through a complex
system, more Insulin is secreted and reduction in 'peripheral insulin resistance',
which is the hallmark of Type 2 Diabetes
Lifestyle
Only with lifestyle changes can any Bariatric surgery be effective. These include
regular exercise, healthy eating, stopping smoking and avoiding high calorie foods.
Who benefits from an Omega loop Gastric Bypass?
People who are committed to lifestyle changes and psychologically prepared with a;
- BMI >40
- BMI >35 with comorbidites (Diabetes / Obstructive Sleep Apnoea / Joint disease)
- Certain international Guidelines include BMI >30 and recent-onset type 2
Diabetes
Lower BMI's considered in case-by-case basis
People who have attempted several months of weight loss without desired results and
no
contraindication to surgery (liver / kidney failure, critical heart disease)
What are the benefits of an Omega loop Gastric Bypass?
- Weight loss of between 65-75% excess body weight (sometimes higher)
- Potential resolution of comorbidities
- Type 2 Diabetes (approx 90%)
- High blood pressure
- Obstructive sleep apnoea
- Halt deterioration of weight related conditions
- 40% reduction in all cause mortality (mostly due to improvement of Diabetes,
Cardiovascular risk factor and Cancer reduction)
- A BMI >40 is equivalent to smoking in shortening ones life expectancy
Contraindications to an Omega loop Gastric Bypass
- Not psychologically prepared for lifestyle changes
- Non-compliance to follow-up / medications
- Certain medical conditions
Preoperative Cares
- Continued weight loss / lifestyle changes.
- Stop smoking.
- Reduce Alcohol intake. Postoperatively it is recommended to avoid alcohol
completely for
6 months.
- Stabilisation / optimisation of co-morbidities (Diabetes / High blood pressure)
- 2-3 weeks before surgery you commence OPTIFAST diet, a very low-calorie diet
(VLCD) that
is <800kcal per day that completely replaces your meals / diet (Nutritionally
complete)
This achieves further weight loss, and deceases the size of your liver improving
surgical access and safer surgery with less complications
Dietician Review
All patients will be assessed by our Dietician
This is to:
- Optimise preoperative weight loss
- Education surrounding a healthy diet
- Prepare yourself for the dietary changes necessary after surgery
Psychologist Review
All patients will be assessed by our
psychologist. This is routine and been shown to improve one's understanding around
the operation and the post-operative effects on your life
Risks of surgery
- Death - < 1 in 400 patients
- Bleeding - 3% chance of blood transfusion
- Conversion - <2% risk of a large scar
- Injury to bowel - <1%. From the insertion of the laparoscopic
ports
- Leak - 2%. From staple line. This is serious complication. That
may result
infurther surgery and prolonged hospital stay. A leak is the most common
surgical causes for death
- Medical complications - DVT (clots), Heart attacks, Skin
infections, Stroke,
Pancreatitis
Long term concerns
- Bile reflux symptoms - 10-20% patients experience
reflux symptoms due to the increased presence of bile within the stomach pouch
refluxing up the oesophagus
- Smaller meals - Smaller stomach volume after surgery
- Dehydration - Due to smaller volume fluid drunk
- Excessive weight loss - Slow sustained weight loss best
- Nutritional Deficiencies - Multi vitamins and Vit B12
injections required. Calcium, Iron and Vitamin B12 are most common deficiencies.
Malnutrition from vitamin deficiencies are more common then after Roux-en-Y
gastric
Bypass
- Psychological - Depression, anxiety and adjustment disorders
can occur in the
longer term
- Gallstones - Not infrequently stones develop following
Bariatric
surgery. Management is dictated by symptoms
- Abdominal bloat / vomiting - Due to
various causes. Can be due to "dumping" of food into small intestine, internal
scars, or angulation of the sleeve. The Latter may require intervention (Surgery
or
Endoscopic dilation)
- Hernia - Through surgical scars ("port site" hernia) or through
defects created by forming the "Bypass"
- Conversion to Roux en Y gastric bypass -
Study's have shown that 7-10% of patients have a further operation to convert an
Omega loop bypass to a Roux-en-Y bypass within 5 years. This is generally due to
reflux of bile into oesophagus ("Heartburn")
Postoperative Cares
- Hospital Stay - 2 nights
- Clinic review - 1-week post-op, 4 weeks post-op, 3 months
post-op
- Diet - Optifast for 3 weeks, Soft diet from weeks 3-6 weeks,
Lite diet from 6
weeks
- Dietician and Nurse Specialist input