Roux-en-Y Gastric Bypass
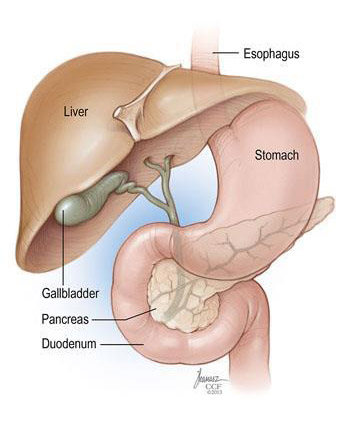
A Gastric Bypass is a major operation to create a small stomach pouch and rearrange the small
bowel to partially "bypass or delay" the food eaten from being in
mixed with the digestive enzymes. This results in
both malabsorptive and restrictive changes that results in weight loss and
generally improvement in various comorbidities (such as diabetes and hypertension).
A Roux-en-Y Gastric Bypass is a major laparoscopic operation, and requires lifestyle
changes to maximise its results.
How does a Roux-en-Y Gastric Bypass work?
Restrictive
The majority of the stomach is disconnected forming a small pouch at the top of the
stomach. This measures approximately 50ml. This results in less food eaten and
'early satiety', which is the sensation of feeling full and satisfied after eating
smaller volumes and thus less calories consumed.
Malabsorptive
This pouch is reconnected to a segment of small bowel in a "Roux-en-Y"
configuration, resulting in the nutrients eaten not being in contact with the enzymes
required for breakdown and digestion until further down the gastrointestinal tract
(The "gut"). Therefore the body has less time to absorb these calories before
passage into the large bowel / colon
Other changes
Metabolic and Hormonal changes occur after the operation. These are changes in
the hormones and signals sent from the remaining stomach to the body. These
signals cause the body to secrete less hormones, that in turn 'turn down' your
appetite. Your body responds by controlling glucose and fats better within the blood
stream. Through a complex system, more Insulin is secreted and reduction in
'peripheral insulin resistance', which is the hallmark of Type 2 Diabetes
Lifestyle
Only with lifestyle changes can any Bariatric surgery be effective. These include
regular exercise, healthy eating, stopping smoking and avoiding high calorie foods.
Who Benefits from a Roux en Y gastric bypass?
People who are committed to lifestyle changes and psychologically prepared with a;
- BMI >35
or
- BMI >30 with comorbidities (Diabetes / Obstructive Sleep Apnoea / Joint
disease)
- Who has attempted several months of weight loss without desired results
and no contraindication to surgery (liver / kidney failure, critical heart
disease)
What are the benefits?
- Weight loss of between 80-85% excess body weight (sometimes
higher)
- Diabetes (approx 70%)
- High blood pressure
- Obstructive sleep apnoea
- Halt deterioration of weight-related conditions
- 40% reduction in all-cause mortality (mostly due to the improvement of
Diabetes, Cardiovascular risk factor and Cancer reduction)
- A BMI >40 is equivalent to smoking in shortening one's life expectancy
What are the contraindications?
- Not psychologically prepared for lifestyle changes
- Non-compliance to follow-up / medications
- Certain medical conditions
- Smoker
Preoperative care
- Continued weight loss / lifestyle changes.
- Stop smoking.
- Reduce Alcohol intake. Postoperatively it is recommended to avoid
alcohol completely for 6 months
- Stabilisation / optimisation of co-morbidities (Diabetes / High blood
pressure)
- 3 weeks before surgery you commence OPTIFAST diet, a very low-
calorie diet (VLCD) that is <800kcal per day that completely replaces your
meals/ diet (Nutritionally complete)
This achieves further weight loss and deceases the size of your liver improving
surgical access and safer surgery with less complications
Dietician Review
All patients will be assessed by our Dietician
This is to:
- Optimise preoperative weight loss
- Education surrounding a healthy diet
- Prepare yourself for the dietary changes necessary after surgery to
improve weight loss and longevity of effect
Psychologist Review
All patients will be assessed by our psychologist. This is routine and been shown to
improve one's understanding around the operation and the post-operative effects on
your life
Risks of surgery
- Death - <1 in 600 patients
- Bleeding - 1% chance of blood transfusion. May require a return to
surgery
- Conversion - <1% risk of a large scar
- Injury to bowel - <1%. From the insertion of the laparoscopic
ports
- Leak - 1%. From the staple lines and anastomosis (Bowel 'joins').
This
is a serious complication. That may result in further surgery and
prolonged hospital stay. This is the complication that increases the risk of
death.
- Vomiting / dehydration - <5%. Due to small stomach volume
- Narrowing of the join / anastomosis - 5% may need a stretch with a
gastroscopy between week 4-8 post op
- Medical complications - DVT (clots), Heart attack, Skin infection,
Stroke, Pancreatitis
Long term concerns
- Dehydration - Due to smaller volume fluid drunk, and fluid shifts
in the
bowel.
- Excessive weight loss - slow sustained weight loss best.
- Nutritional Deficiencies - Multi vitamins and Vit B12 injections
required. Calcium, Iron and Vitamin B12 are most common deficiencies.
- Psychological - Depression, anxiety and adjustment disorders can
occur in the longer term.
- Gallstones - Not infrequently stones develop following Bariatric
surgery.
management is dictated by symptoms.
- Abdominal bloat / vomiting - Due to various causes. Can be due to
"dumping" of food into the small intestine, internal scars, or angulation of
the sleeve. The latter may require intervention (Surgery or Endoscopic
dilation).
- "Dumping Syndrome" - A constellation of symptoms (usually
sweating / pain / feeling faint) following the rapid transit of food into the small
bowel. Due to either loss of fluid into the small bowel (Early) or low blood
sugar (Late). Managed by avoiding sweet foods / dietary modification and
increasing fluid intake.
- Hernia - Through surgical scars. "Port site" hernia or "Internal
Hernia"
through small openings created during bypass