The Gastrointestinal tract (gut) is a complex system of hormones, enzymes and feedback-systems that control the absorption of food, the bodies response to and desire for more food (Satiety). Surgery alters the gut to achieve both weight loss and better metabolic control of the absorbed calories / glucose. This is achieved by RESTRICTIVE, MALABSORPTIVE (or a COMBINATION OF RESTRICTIVE / MALABSORPTIVE) types of surgery.
Most absorption of food (Calories, elements and vitamins) occurs in the small bowel. The large bowel is almost mostly solely for fluid absorption. Various parts of the small bowel are more designed to absorb different parts of your diet (i.e. Calcium in Duodenum, vitamin K in Terminal ileum) and secrete a number of hormones to control digestion and feed-back to the brain.
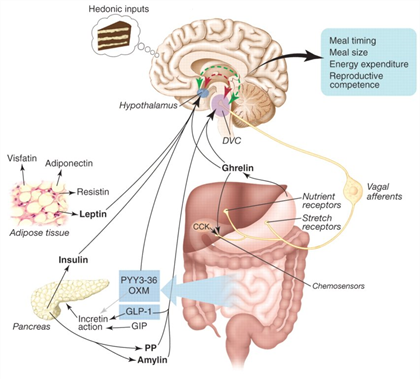
The Stomach is a reservoir that can hold over 1000ml, this enables us to comfortably have large meals (i.e. three square meals a day). Weight loss surgery creates a smaller gastric 'pouch' or 'sleeve'. This is typically 50-100ml in volume and significantly decreases the volume one can consume at once. When this new stomach is filled up at low volumes, it signals through nerves and hormones to the brain to stop eating and the body and brain feel satisfied and “full”. Patients do not desire to eat more (Satiety) due to the brains response to Ghrelin. Ghrelin is known as the “hunger hormone”.
Weight loss surgery re-arranges the internal plumbing of the small bowel to delay the mixing of eaten food with the bile and enzymes required for its digestion. This delay in mixing means that there is less time in the small bowel for this digestion to occur and less calories absorbed. Typically this mixing is delayed by 100-150cm (the typical small bowel length ranges from 300cm - 600cm).
Weight loss surgery causes alteration in various hormones that result in the body behaving differently to ingested food / calories. This is not completely understood, but the most commonly described immediate change is the loss of peripheral insulin resistance seen in type 2 Diabetics. Within days of surgery a large number of Diabetic patients have better control of their blood sugar levels as a result of the body responding to insulin more effectively and lowering blood sugar levels. Other metabolic benefits seen are improved blood pressure and lipid profile through complex feed-back loops.