POST OP PROTOCOL
Day 0 (day of surgery)
• May have sips of water up to 30mls per hour
• Encourage mobilisation
• IV Omeprazole as charted
• STOP all diabetic medication
• Regular anti-emetic as charted
• Strict fluid balance – show patient how to record this themselves
• Sub-cut Clexane as charted
• TEDS should still be in place from admission
Day 1 post op
• Start sips of water 30ml/hr. – if well tolerated increase to 60ml/hr. by mid-day
• Stop IV fluids once tolerating 60ml per hour
• Strict fluid balance – patient to record fluids themselves
• Can change to oral medication – these must be crushed or capsule opened
IV Omeprazole change to oral Pantoprazole 20mg daily
Contents swallowed only, capsule to be discarded
• If tolerating 60mls per hour later in the day then progress to dilute Optifast (or similar) into 400mls of fluid)
• Remind patient to re-read the dietitian information
Day 2 post op (if not discharged day 1)
• Increase oral fluids to 100mls per hour if tolerated and introduce dilute Optifast as above
• Can begin Berocca performance (dilute) once daily or wait until discharge – Optifast is more important at this stage
• Aim for discharge
Discharge plan
• Paracetamol (dissolvable or suspension) Q4-6H for at least 48hrs
• Pantoprazole 20mg PO daily for the next 12 months due to risk of developing a gastric ulcer. Crush until 3-4 weeks post procedure
• Centrium Advance 50+ (x2 per day) once on pureed diet (2-3 weeks post procedure) or Celebrate Bariatric Multivitamin (chewable, one per day) on discharge
• Crush all usual medications (or open capsules) for at least 3 weeks
• Dietitian sheets and vitamin supplement sheets given to patient with contact details if any problems arise
• Bowel management (preventative promoted) e.g. alpine tea or Phloe tablets
• Strictly no NSAIDs after Gastric Bypass
• Clinic review approx. 1 week post op
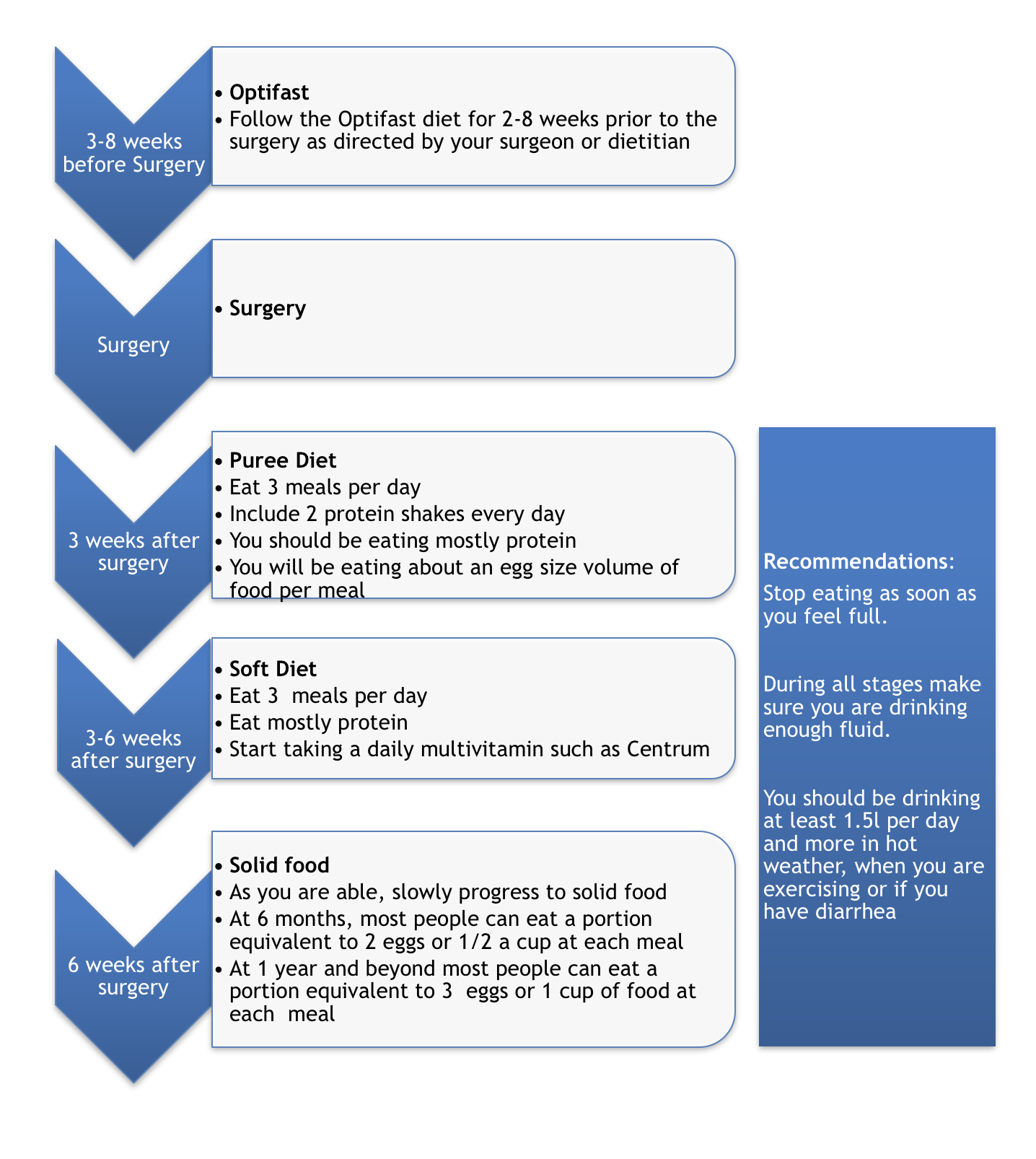
Week 1 = Liquids
For the first day after surgery, you’ll only be allowed to drink clear liquids.
Once you’re handling clear liquids, you can start having other liquids, such as
- Optifast (or similar)
- Broth
- Unsweetened juice
- Decaffeinated tea or coffee
- Milk (skim)
- Sugar-free gelatin or popsicles
Aim for 1.5 – 2.0 litres per day
All drinks should be low in sugar
Weeks 2-3 = Pureed foods
After 1 week of tolerating liquids, you can begin to eat strained and pureed (mashed up) foods. The foods should have the consistency of a smooth paste, pudding or a thick liquid, without any solid pieces of food in the mixture. V-8 juice and first-stage baby foods, which do not contain solids, are also convenient options.
As you start to include purees into your diet, it’s important not to drink fluids while you eat.
You can eat three to six small meals a day. Each meal should consist of 4 to 6 tablespoons of food.
- Eat slowly — about 30 minutes for each meal
Choose foods that will puree well, such as:
- Lean ground meat, poultry or fish, cottage cheese, soft scrambled eggs , yogurt, white fish, cottage cheese, ricotta, cooked cereal, soft fruits and cooked vegetables (applesauce, bananas, canned fruits , peaches, apricots, pears, pineapples, melons), strained cream soups
Blend solid foods with a liquid, such as:
- Water, Skim milk, Juice with no sugar added, Broth
Practical tips to help meet Nutritional Requirements at Pureed Stage:
- Each meal should include a high protein food item
- Protein shakes should be included to help ensure an adequate protein intake and protein powder can be added to meals to increase the protein content
Spicy seasonings may irritate the stomach, so avoid these completely or try them one at a time.
Avoid fruits that have lots of seeds, such as strawberries or kiwifruit. You should also stay away from foods that are too fibrous to liquefy, such as broccoli and cauliflower.
Weeks 4-5 = Soft foods
After a few weeks of pureed foods you can start soft diet (generally week 4). They should be small, tender and easily chewed pieces of food.
You can eat three to five small meals a day. Each meal should consist of one-third to one-half cup of food. Chew each bite until the food is pureed consistency before swallowing.
Soft foods include:
- Ground lean meat or poultry, Flaked fish, eggs, Cottage cheese, cooked or dried cereal, rice, canned or soft fresh fruit, without seeds or skin, cooked vegetables, without skin
Include 1 protein shake per day as part of fluid intake
- Optifast® shakes / soups / desserts (Pharmacies, PharmacyDirect.co.nz)
- Red8 Protein Plus, Whey or Soy Protein (Health 2000 stores, PharmacyDirect.co.nz)
- Balance, 100% Whey Protein (Health 2000 stores, PharmacyDirect.co.nz)
- Clean Lean Protein Pea (Health 2000 stores, Hardys, PharmacyDirect.co.nz)
>6 Weeks = Solid foods
After about 6 weeks on the gastric bypass diet, you can gradually return to eating firmer foods. Start with eating three meals a day, with each meal consisting of 1 to 1-1/2 cups of food. It’s important to stop eating before you feel completely full.
Depending on how you tolerate solid food, you may be able to vary the number of meals and amount of food at each meal. Talk to your dietitian about what’s best for you.
Try new foods one at a time. Certain foods may cause pain, nausea or vomiting after gastric bypass surgery.
Foods that can cause problems at this stage include:
- Breads, carbonated drinks, raw vegetables, cooked fibrous vegetables, such as celery, broccoli, corn or cabbage, tough meats or meats with gristle, red meat, fried foods, highly seasoned or spicy foods, nuts and seeds and popcorn
Avoid
- Avoid alcohol 6 months, fizzy drink 3 months, chewing gum 1-3 months
- limit caffeine to 1 Café coffee per day (so long as you are drinking >1.5l/day)
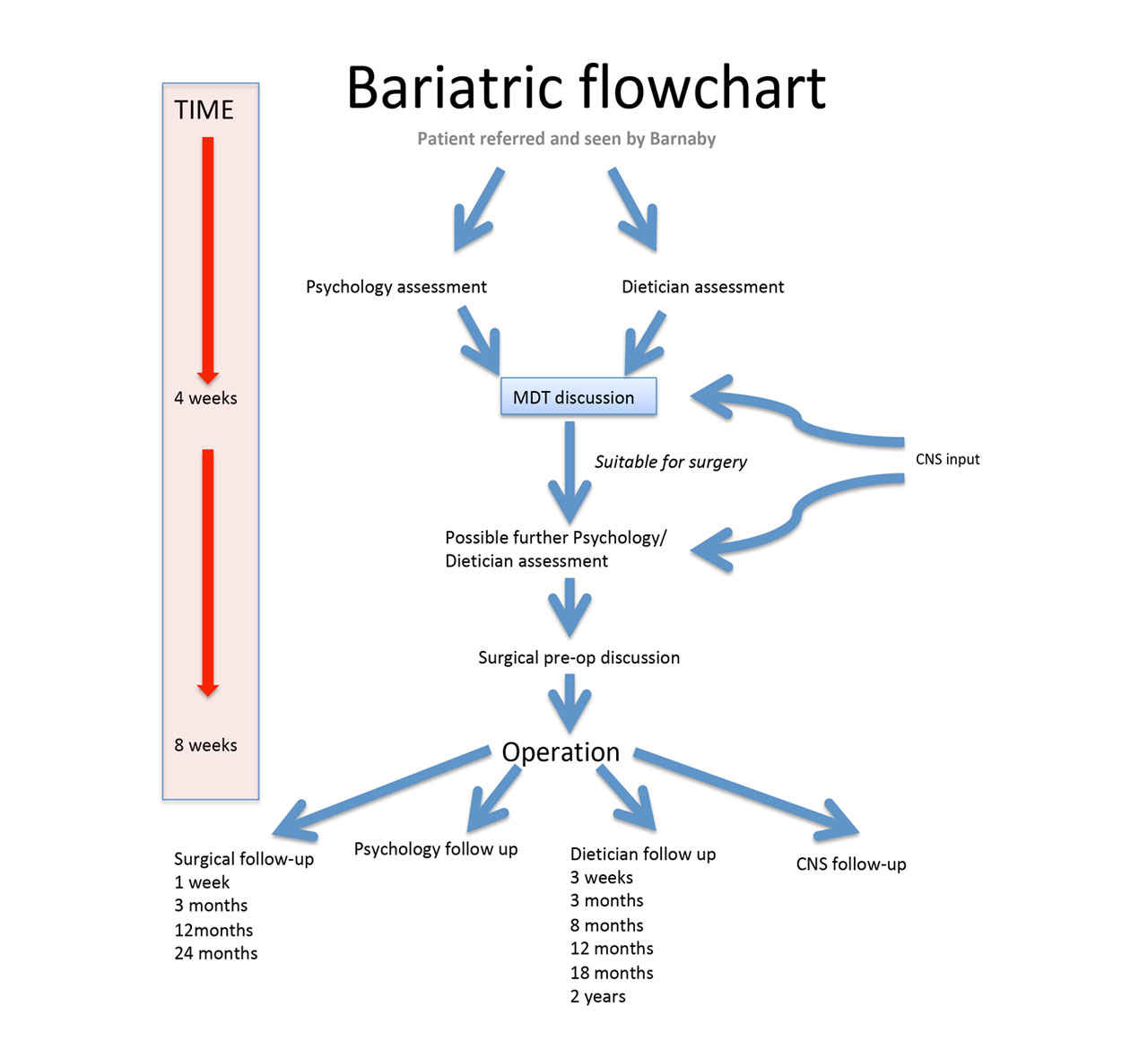
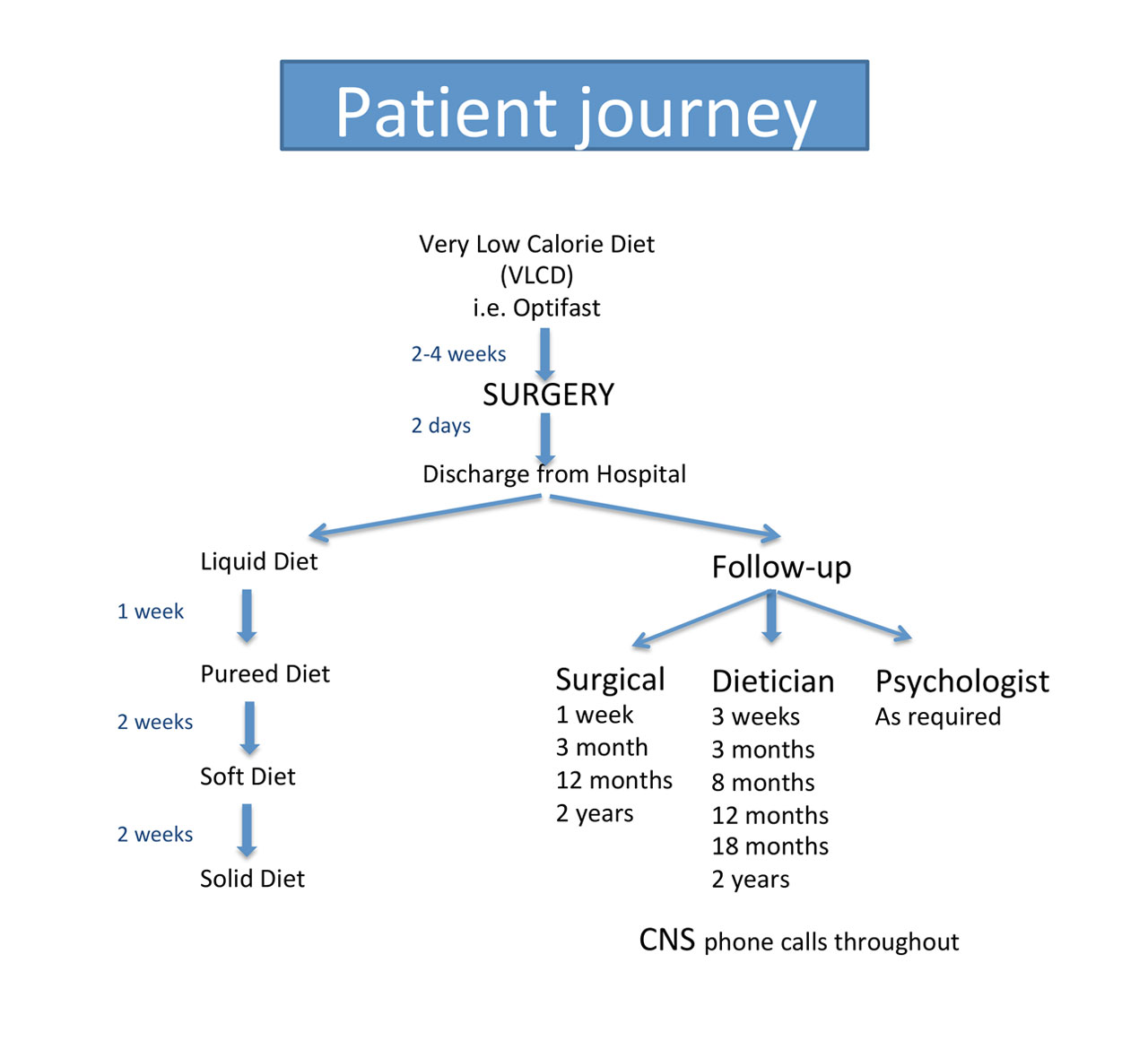
Post Operative Follow-up
Surgical review
- Week 1-2
- Week 3
- 12 months following surgery
Stop Omeprazole at 6 months
DEXA (bone density scan) at 1 and 5 Years
Dietician post op
- Week 3
- 3 months
- 8 months
- 12 months
- 18 months
- 2 years
Psychologist/ Group Sessions
Long Term Considerations
Eat Slowly
- Chew your food 20 times before swallowing
Ensure you eat enough protein
- Eat your protein before your carbohydrates
Avoid liquids with meals (do not drink within 30 mins before or after meals)
Exercise at least 30mins 5 times per week
Avoid alcohol 6 months
- Your tolerance to alcohol may be significantly lower postoperatively
Try to limit caffeine in taking to 1-2 cups per day
Avoid pregnancy for 12 months post surgery
- Use contraception during this waiting period (oral contraception may be less effective)
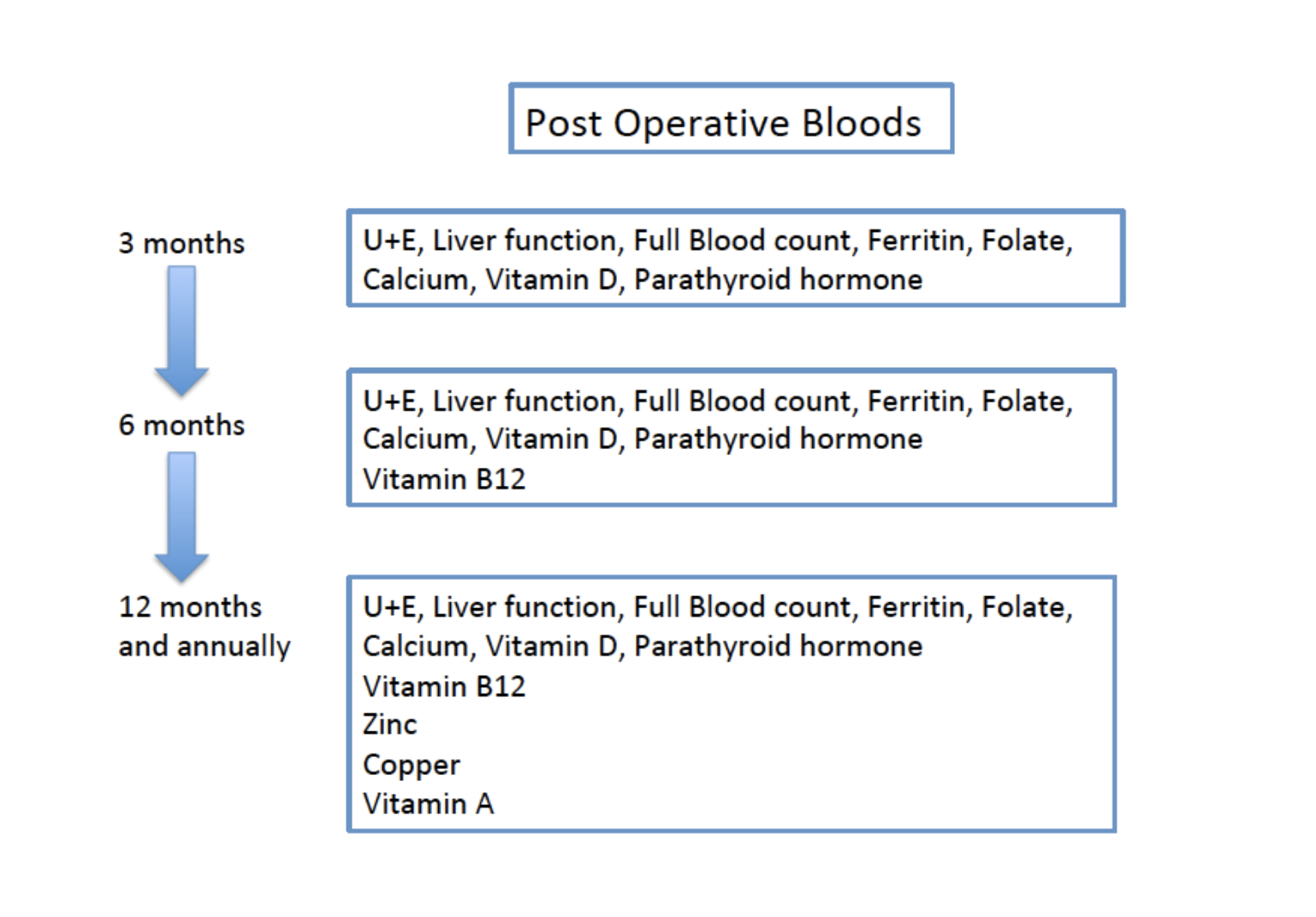
- Get regular blood tests to look for nutritional deficiencies. You may need additional supplements
- See a Dietician to help regulate weight gain during pregnancy
Always carry drink bottle on your person
- To sip clear fluids over the course of the day
Try to carry/ have handy a protein bar (or similar) to eat if feeling fatigued/ low blood sugar
We strongly recommend that you NEVER smoke postoperatively
- Smoking is the main contributor to Gastric pouch ulceration
Avoid Non-Steroidal Anti Inflammatory pain relief (NSAID’s)
- Increase Gastric pouch ulceration
Continue Multivitamin/ Calcium/ Vitamin D tablets lifelong
Monitor vitamin B12 with 6 monthly blood tests
- You may require a vitamin B12 injection if low
Dumping syndrome can occur after eating a high sugar meal/sweets
- Can make you feel unwell (Dizziness/pain/flushes/cramps/diarrhoea).
- This is self limiting/ Not harmful
- Immediately after eating, or delayed by 2-3 hours
- Managed by avoiding sweet/ high sugar foods and increasing fluid intake
Constipation can be an issue. Laxatives may be required as oral fibre intake may be low.
If at any stage you feel unwell postoperatively it is important to contact us (especially in the first week postoperatively)
Such as;
- FEVERS/ SWEATS/ DEHYDRATION/ SEVERE ABDOMINAL PAIN/ SIGNS OF INFECTION
Mr Barnaby Smith
Ph 571 5548
Mob 021988961
Email info@barnabysmithsurgical.co.nz